Human anti-Rhesus immunoglobulin rho d. Camrow - official instructions for use
Manufacturer: PJSC "Biopharma" Ukraine
PBX code: J06B B01
Farm group:
Release form: Liquid dosage forms. Injection.

General characteristics. Compound:
Active ingredients - immunoglobulin - 300 mcg (antibody titer 1:2000);
excipients - glycine (glycocol, aminoacetic acid), sodium chloride.
Main properties: the drug is an immunologically active protein fraction of serum or blood plasma of immunized donors (or reimmunized donors), tested for the absence of antibodies to HIV-1, HIV-2, hepatitis C virus and surface antigen of the hepatitis B virus, purified and concentrated by fractionation ethyl alcohol, which has undergone the stage of viral inactivation using the solvent-detergent method, with a high content of anti-Rh o (D) antibodies. The protein content in 1.0 ml of the drug is from 0.09 g to 0.11 g. Transparent or with slight opalescence, colorless or yellowish liquid. During storage, a slight sediment may appear, which disappears with shaking. The drug does not contain preservatives or antibiotics.
Pharmacological properties:
The active basis of the drug is immunoglobulin specific to the Rho (D) antigen. The antibody titer in 1 dose of the drug is at least 1:2000 (300 μg of immunoglobulin), which is determined using the Coombs test. The drug prevents Rh-sensitization of Rh-negative women, possible as a result of the entry of Rho (D)-positive fetal blood into the mother’s bloodstream at the birth of Rho (D)-positive children, during termination of pregnancy (both spontaneous and artificial), in the case of , when injured abdominal cavity during pregnancy.
Indications for use:
The drug is used:
For prophylaxis during the prenatal period in Rh-negative women who are not sensitized to the Rh o (D) antigen;
For prevention in postpartum period in Rh-negative women who are not sensitized to the Rh o (D) antigen, i.e. have not developed Rh antibodies (subject to the first pregnancy and the birth of a Rh-positive child, whose blood is compatible with the mother’s blood according to the ABO blood groups);
During artificial termination of pregnancy in Rh-negative women, who are also not sensitized to Rh o (D) antigen, in the case of Rh-positive blood of the husband;
In case of miscarriage or threatened miscarriage at any stage of pregnancy;
When performing amniocentesis;
In case of injury to the abdominal organs during pregnancy.
Important! Get to know the treatment
Directions for use and dosage:
When applying, the following criteria must be taken into account:
· The mother must be Rh negative and must not already be sensitized to the Rh o (D) antigen;
Her child must be Rh positive and have negative result direct antiglobulin test. If the drug is given before birth, it is essential that the mother receives another dose of the drug after the birth of her Rh-positive baby within 72 hours of delivery. If it is determined that the father is Rh negative, there is no need to administer the drug.
Immunoglobulin is administered in one dose (300 mcg) intramuscularly once:
When carrying out prophylaxis in the prenatal period at approximately 28 weeks of pregnancy. After this, another dose (300 mcg) must be administered, preferably within 72 hours after birth, if the born baby is Rh positive.
When carrying out prophylaxis in the postpartum period during the first 72 hours after birth;
At induced abortion, interruption ectopic pregnancy- immediately after the end of the operation. If the pregnancy is more than 13 weeks, a single dose is recommended; if the pregnancy is terminated at less than 13 weeks, a single mini-dose of immunoglobulin (approximately 50 mcg) may be used;
In case of miscarriage or threatened miscarriage - at any stage of pregnancy;
When performing amniocentesis or receiving injuries to the abdominal organs during the second and/or third trimester of pregnancy, it is recommended to administer one dose of the drug immediately after the end of the operation. If amniocentesis or trauma to the abdominal organs requires administration of the drug at 13-18 weeks of pregnancy, another dose (300 mcg) should be administered at 26-28 weeks.
One dose of the drug (300 mcg) with an AT titer of 1:2000.
Features of application:
It is prohibited to administer the drug intravenously!
Use under medical supervision. Before administration, ampoules with the drug are kept for 2 hours at room temperature (20±2) ºС. The drug cannot be stored in an open ampoule. After the expiration date, the use of the drug is unacceptable. Immunization of women with live vaccines should be carried out no earlier than 3 months after the administration of human Rh o (D) immunoglobulin.
Use during pregnancy and lactation. See sections “Indications for use”, “Method of administration and dosage”.
Children. The drug should not be administered to newborns! Children born to women who received the drug before birth may receive weakly positive results from direct tests for the presence of antiglobulin at birth. It is possible to detect antibodies to Rh o (D) obtained passively in the mother's blood serum if screening tests for antibodies are carried out after prenatal or postpartum administration of human anti-Rh o (D) immunoglobulin.
Side effects:
As a rule, there are no reactions to the administration of immunoglobulin. In rare cases, local reactions may occur in the form of hyperemia and an increase in temperature to 37.5 o C during the first day after administration. The drug may cause allergic reactions in some patients with altered reactivity. different types, and in rare cases - . In this regard, patients who received the drug should be under medical supervision for 30 minutes. Phenomena are possible.
Interaction with other drugs:
Possible combination with other specific medicines.
Contraindications:
The administration of immunoglobulin is contraindicated in persons with a history of severe allergic reactions to the administration of human blood protein products. Administration of the drug is contraindicated for Rh-positive postpartum women, as well as Rh-negative postpartum women sensitized to the Rh o (D) antigen, in whose serum Rh antibodies are detected.
For patients suffering from allergic diseases, or having a history of them, antihistamines are recommended on the day of immunoglobulin administration and for the next 3 days.
Overdose:
Not studied.
Storage conditions:
In a dry place, protected from light, at a temperature of 2°C to 8°C. Keep out of the reach of children.
Vacation conditions:
On prescription
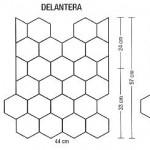
Package:
1 dose (300 mcg of immunoglobulin with an antibody titer of 1:2000) per ampoule. 1 or 3 or 5 ampoules per pack.
Immunoglobulins (Ig) are a group of serum proteins, heterogeneous in a number of ways, most of them are located in the region of γ-globulins during electrophoresis, and some are located in the region of the beta-globulin fraction.
Immunoglobulins are heterogeneous in their physicochemical and biological properties and also have structural differences. The WHO Expert Committee has developed a classification of human immunoglobulins, according to which they are divided into classes A, D, E, G, M.
Immunoglobulins A
IgA is usually found in immune sera in low concentrations. In structure and properties they differ from IgG and IgM. This is a heterogeneous group of proteins, located during electrophoresis in the region of beta globulins. It consists of components that differ in mass, sedimentation constant -7S, 9S, 11S and 19S. The 7S IgA molecule contains two active centers, which have a greater affinity for the antigen than 7S IgG antibodies of the same specificity.
IgA contains light chains that are identical in immunochemical properties to the light chains of IgG and IgM of the same type. The H-chains of IgA differ significantly from those in IgG in their size and structure.
IgA makes up about 20% of the total number of immunoglobulins and is the main secretory immunoglobulin. Contained in colostrum, tear fluid, bile, intestinal juice, sputum. Secretory immunoglobulins A are important in protection against intestinal and respiratory infections and determine the severity of local immunity. The development of immunity in respiratory diseases is associated with this Ig class; impaired IgA synthesis is accompanied by the development of respiratory tract diseases.
In the mucous membrane of the digestive apparatus, plasma cells predominate, synthesizing secretory IgA, responsible for the human immune defense against intestinal invasion.
IgA of secreted fluids (bronchi, intestines, saliva) are identical to each other, but differ from IgA of blood serum by an additional chain (I).
Immunoglobulins D
These proteins differ from other classes of immunoglobulins in the structure of the H-chains and biological properties. Immunoglobulins D are present in biological fluids in very low concentrations and constitute about 1% of all Igs. Their molecular weight is about 180,000.
IgD does not have the property of fixing complement and does not pass through the placenta. Its role in the body is extremely insufficiently studied. IgDs are believed to be related to immunological memory.
Immunoglobulins E
The IgE group includes antibodies of the reagin type, responsible for the immediate type. They do not pass through the placenta, do not fix complement, and do not tolerate cutaneous passive anaphylaxis with blood serum. They are characterized by the ability to sensitize human skin, therefore one of the methods for their detection is the Prausnitz-Küstner passive transfer reaction. They also sensitize the mucous membranes of the nose, eyes, and respiratory apparatus. In healthy individuals their levels are very low. With allergies, the IgE level increases 4-30 times. They contain 20% light chains, 80% heavy chains (E-chains heavy chains). IgE 8S sedimentation constant. In an electric field they migrate with the y- and beta-fraction of serum globulins at pH 8.6.
Reagins are non-precipitating antibodies, which makes their detection difficult. There are a number of methods for determining IgE. The reagin-allergen complex is combined with a substrate, which is detected by radiological methods. Both the total total amount of IgE and the level of IgE against a particular allergen are detected (specific reagins). A number of other methods are also used (reaction of degranulation of basophilic granulocytes, degranulation of tissue basophils).
Reagins are bivalent. At one end they are connected by heavy chains (Fc) to the cell, and at the other (Fab) to the allergen. One allergen molecule combines with two reagin molecules.
Reagins can also connect with smooth muscle cells of organs (bronchi, intestines, uterus), connective tissue and blood (tissue basophils, basophilic granulocytes, lymphocytes), with capillary endothelial cells and other tissues. These cells have receptors for Fc IgE. IgE is formed only in humans, but can also be fixed by animal tissue cells. Reagins are also found in the secretions of the nasal mucosa of patients with hay fever; with reactions of the reagin type, eosinophilic granulocytes appear in the bronchial secretions.
After the discovery of IgE as the antibody responsible for the immediate type of allergic reactions, it was long believed that other types of Ig are not involved in the mechanisms of allergy, in particular in the pathogenesis of asthma. However, evidence has gradually accumulated that immunoglobulins of other classes play a significant role.
Immunoglobulins of various classes have significant physicochemical and structural differences that determine their biological properties.
The entire diversity of properties and biological functions of antibodies is determined by the Fc and Fab fragments of immunoglobulins of various classes. The Fab fragment, the carrier of the active center, determines the avidity of antibodies, that is, the degree of their ability to bind to the antigen. Thus, immunoglobulin G and immunoglobulin M differ in their avidity depending on the type of antigen. For example, corpuscular antigens interact more strongly with IgM, which is explained by the polyvalency of this type of immunoglobulin. Antigens that are simpler in structure (protein, polysaccharide) bind more strongly to IgG, the active center of which is characterized by greater avidity.
Structural differences in the Fc fragments of different classes of immunoglobulins determine the unequal properties of antibodies to one antigen, their different abilities fix complement, neutralize toxins, permeability through biological membranes, etc. For example, the ability to fix complement plays a very important role both in the implementation of the body’s defense reactions and in the participation of complement-fixing antibodies in the formation of immunopathological processes.
The Fc fragment has a cytotropic region, due to which immunoglobulins attach to cells (antibody homocytotropy); this may cause the corresponding cells to react. This kind of cell reaction ends with the release of biologically active substances such as histamine, which occurs in immediate type allergies.
This homocytotropy is inherent in IgE, which mainly determines the pathogenesis of allergic diseases.
Antibodies belonging to different classes of immunoglobulins play different roles in the formation pathological process. The study of immunoglobulins is very important in assessing the state of immunological reactivity and especially in diagnosing diseases with impaired immune system.
An important point in the study of immunoglobulins was the creation of simple quantitative methods based on the use of monospecific sera. The most widely used method is radial diffusion.
Most studies usually use the definition of three classes of immunoglobulins - G, M, A. Immunoglobulins D, E are determined less frequently. IgE research is carried out using special techniques.
The normal ratio of immunoglobulins is: immunoglobulin G -85%, immunoglobulin A-10%, immunoglobulin M -5%, immunoglobulin D and immunoglobulin E - less than 1%. The level of IgG in newborns is 80% or more of the level in adults. In the elderly, on the contrary, an increase in the level of all classes of immunoglobulins is observed.
When assessing the humoral component of immunity, it is important not only to determine the amount of individual classes of immunoglobulins, but also to identify the content of antibodies to a specific antigen.
The concentration of immunoglobulins reflects the state of the immune organs, the strength of the antigenic stimulus, but there is no direct relationship between the content of immunoglobulins and the level of antibodies to a specific antigen.
Great importance is attached to the study of the ratio of immunoglobulins in bronchial asthma. At the same time, many authors note the presence of disimmunoglobulinemia, the severity of which depends to a certain extent on the form and severity of the disease. However, there is no clearly defined pattern in this regard.
Many researchers note an increase in the levels of immunoglobulins of all classes in infectious-allergic asthma. A number indicate significant fluctuations in the level of various classes of immunoglobulins. This heterogeneity is explained by the wide variety of patient populations examined, the variety of etiology and pathogenesis of the disease and its severity.
Data on IgE levels in asthmatics are of great interest. There is a sharp increase in the atopic form of asthma, less pronounced in the infectious-allergic form of the disease. consider a high level of immunoglobulin E in the blood with a simultaneous decrease in IgA as a poor prognostic sign.
As for immunoglobulins in bronchial secretions, the literature information is very diverse. Indicated by more high level IgA and IgG in bronchial washings of patients with asthma compared with their content in patients with bronchitis. Allergists explain this by hypersecretion of Ig in bronchial asthma. Other authors, on the contrary, note a decrease in the content of immunoglobulins in bronchial secretions. It can be assumed that the fact of an increase in IgG levels with a decrease in IgM is explained by the duration of antigenic exposure.
Immunoglobulins G
The most studied class is IgG, which makes up the bulk of immunoglobulins in adults (0.8-68 g/l). IgG includes antibodies against many antigens, which determines their important protective value.
Using proteolytic degradation methods, doctors deciphered the structure of the IgG molecule. As it turned out, immunoglobulins G consist of 2 light (L-chain) and 2 heavy (H-chain) polypeptide chains connected by disulfide (-S-S-) bridges, as well as less strong covalet bonds. The L chains are identical in all classes of immunoglobulins; the main structural differences in Ig are localized in the H chains. More detailed studies of the H-chains made it possible to identify four subclasses and isotypes within IgG. IgG subclasses are divided according to their action and specificity. The sedimentation rate of IgG is 7S, molecular weight is 160,000, consists of 1330 amino acids. The immunoglobulin G molecule has two centers of the same structure, which are the working part of the molecule and are also called combining participants.
From IgG, using proteolytic enzymes, one section can be separated, including two parts of heavy chains that do not have an active center, the Fc fragment (Fragment constant). The rest of the molecule is divided into two Fab fragments (Fragment antigen binding), which can bind antigen and include one light chain and part of a heavy chain. Each Fab fragment has one active center, which determines the specificity of antibodies. The active center, or otherwise combining region, is formed by a small number of amino acids (about 15) and gives the molecule specificity and unique variability. This active site is related to both chains.
The variability of the amino acid composition in the active site of the Fab fragment ensures the formation of a large number of structural variants, complementary to a variety of natural and synthetic antigenic determinants. The constancy of another Fc fragment determines the uniformity of the effector function of a given class of immunoglobulins. IgG is the only immunoglobulin that can cross the placenta.
Immunoglobulin M
Proteins of this class make up 5-10% of serum immunoglobulins. They are macroglobulins, have a molecular weight of 900,000-1,000,000, and during electrophoresis they migrate in the zone of beta globulins. The immunoglobulin M molecule consists of five units, each corresponding to IgG, consisting of 2 heavy and 2 light chains. They are all connected by disulfide bridges. The amino acid composition and antigenic structure of the light chains are similar to those of IgG. IgM heavy chains differ from IgG H-chains in molecular weight, amino acid composition and antigenic structure.
Since the IgM molecule includes five subunits, similar to IgG, one would expect it to have ten active centers, but studies show that in each subunit one of the active centers is inaccessible to the antigen due to spatial difficulties.
IgG is formed during the early stages of immunization with various antigens. When exposed to protein antigens, the synthesis of IgM is quickly replaced by the synthesis of IgG antibodies; if the antigens are of a polysaccharide nature, IgM is synthesized simultaneously with IgG. IgM is not very specific, but in combination with an antigen it has a high activity of fixing complement, which contributes to the rapid destruction of the antigen. This feature is very important in the early stages of infection of the body.
Types of immunoglobulins by nature of action
In addition to assessing individual classes of immunoglobulins, determining the nature of the action of immunoglobulins is also important. In allergic diseases, in addition to reagins, other types of antibodies are also detected (precipitins, hemagglutinins, blockers). They can take part in various allergic processes - bronchial asthma, food allergies, drug allergies, hay fever.
Precipitating antibodies(usually immunoglobulin G), involved in allergic processes, are a component of immune complexes. The latter are localized, penetrating through the vascular wall, in the bronchial alveoli. Activation of complement and release of leukotactic factors lead to the appearance of granulocytes and macrophages. The destruction of the latter releases enzymes and monokines that damage lung tissue, and forms its fibrosis. An inflammatory reaction mediated by biologically active substances develops.
Complement-fixing antibodies participate in the pathogenesis of such allergies as reactions such as “reverse” anaphylaxis, cytotoxic anaphylactic shock, anaphylactic shock in bacterial allergies, tuberculin shock; They also occur in hay fever.
Blocking allergy antibodies are present in the blood of people recovering from allergies. They belong to immunoglobulins G, are heat stable, do not sensitize the skin, and do not cause the formation of precipitates. This type of antibody is formed after specific hyposensitization.
Hemagglutinating antibodies- antibodies that can specifically react with red blood cells connected to the allergen. It has not been conclusively established whether other types of antibodies (reagins or blocking) also have this agglutination property.
Allergic antibodies are specific, but for some types of allergens the specificity is relative, so-called cross-reactions may develop. Reactions between antigen (allergen) and antibody are diverse and lead to various clinical manifestations.
The article was prepared and edited by: surgeonContent
Rhesus conflict entails serious health problems not yet born baby, therefore, it is necessary to respond in a timely manner to the presence of such a pathology. Administration of the drug during pregnancy increases the chances of fetal viability and reduces the list of potential complications during the prenatal period. The pathology is serious, so the woman is under strict medical supervision when carrying a fetus.
What is Rh conflict during pregnancy?
If a woman has a negative Rh factor, she is at risk. This feature of the body does not have a negative impact on her health; problems arise during pregnancy. If the fetus has a positive Rh factor, an Rh conflict develops. This means that the mother's immune system does not yet recognize the cells. born child, as alien, and begins an active fight against them.
The immunity of a pregnant woman produces antibodies-immunoglobulins to such structures, which, penetrating through placental barrier, large-scale destruction of proteins that are not in the morphological composition of the mother’s blood. As a result, jaundice develops in newborns, associated with the breakdown of blood cells (hemolysis). More serious pathologies cannot be excluded, including hydrops fetalis, damage to the brain and heart, and stillbirth. To avoid such complications, the patient must be administered anti-Rhesus immunoglobulin during pregnancy.
When is anti-Rhesus immunoglobulin needed?
For birth healthy child and to exclude Rh conflict, a specific protein is administered to pregnant women with a negative Rh factor. Among other medical indications for the administration of anti-Rhesus immunoglobulin in the absence of the Rh factor, doctors identify:
- spontaneous or intentional termination of pregnancy (abortion);
- abdominal trauma;
- threat of termination of pregnancy at any stage;
- after amniocentesis;
- placental abruption;
- pregnancy with subsequent birth of a child with a positive Rh factor;
- ectopic pregnancy.
How does anti-Rhesus immunoglobulin work?
This protein is isolated from the serum or plasma of donors who have been previously tested for the absence of antibodies to HIV, hepatitis B and C in the blood. When administered, the substance prevents the formation of antibodies to the Rh factor and prevents hemolysis of red blood cells in the fetus. At the discretion of the attending physician, anti-Rhesus immunoglobulin should be administered at 28 obstetric week, but in this case the likelihood of mixing the two bloods even before birth increases significantly.
The optimal time to introduce protein is immediately after the baby is born. This is an effective prevention of hemolytic disease during the next pregnancy. If sensitization is detected (the presence of antibodies to the Rh factor in the blood of the expectant mother) and the Rh factor is positive, the use of anti-Rh immunoglobulin is strictly contraindicated and is not urgently necessary.
Instructions for use of anti-Rhesus immunoglobulin
A single dosage of this medication is determined individually; intravenous administration of serum is completely excluded. IN detailed instructions the application contains the following valuable information for patients at risk:
- The serum should be administered intramuscularly; self-medication is strictly contraindicated.
- Before administering the drug, it is necessary to keep it at room temperature for at least 2 hours (warm under natural conditions).
- To enter the medicine into the body, it is necessary to use a disposable sterile syringe with a wide bore.
- When performing an operation to terminate a pregnancy, the serum must be administered immediately after its completion.
- In the prenatal period, the recommended dose must be taken at the 28th obstetric week - once, then immediately after birth.
- A single dose after successful delivery is 300 or 600 mcg of serum, and it should enter the body of the new mother in the first 48-72 hours.

Contraindications and side effects
This medication completely eliminates the risk of drug interactions, so it is allowed to be administered even during long-term antibiotic treatment. But after receiving a single dose of immunoglobulin in female body doctors do not exclude the possibility of side effects. Among them:
- allergy, skin reactions presented by urticaria, severe itching, burning, rashes and hyperemia skin, less often – acute anaphylactic shock;
- hyperthymia (instability nervous system, represented by unexpectedly high spirits, excessive activity in all areas of life);
- noticeable violations on the part of digestive system, for example, pronounced signs of dyspepsia.
The introduction of this important component into the blood is not allowed for all women with a negative Rh factor. There are medical contraindications presented in the instructions as follows:
- hypersensitivity of the body to active components administered medication;
- prevention of Rh conflict in newborns;
- diabetes in the expectant mother;
- identified sensitization (Rh antibodies detected in the blood).
Special instructions for the use of anti-Rhesus immunoglobulin
The serum cannot be used after the expiration date, non-compliance with the rules and conditions for storing the solution, or if the integrity of the bottle is damaged. Ideally, anti-Rhesus immunoglobulin is a colorless liquid, therefore, if the solution changes color and becomes cloudy, or a precipitate appears in the form of insoluble flakes, the bottle must be disposed of after opening. Vaccination is not possible because it can significantly harm the patient’s health. Other recommendations are presented below:
- Immediately after vaccination, the patient should remain under strict medical supervision. It is possible that side effects may occur, which specialists can effectively manage with medication.
- Within 30 minutes after the injection, an allergic reaction may occur directly at the injection site of the serum. The doctor’s task is to stop anaphylactic shock when it occurs.
- Immunization with a “live” vaccine is carried out no earlier than 3 months after the administration of immunoglobulin.
- If there is a Rh conflict between future parents, it is important to vaccinate when planning pregnancy. This helps increase the chances of having a healthy baby.
- In the presence of an infectious process, it is advisable to undergo an injection of immunoglobulin.
- Rh positive parents or if the father has a negative Rh factor, serum is not required to be administered.

A person is surrounded by bacteria and microbes throughout his life. Many of them living outside do not cause any problems to human health, and some are even beneficial. However, along with harmless microbes, pathogenic microorganisms that provoke viral and infectious diseases. The human body tries to fight them. And this is where immunoglobulins enter the arena.
Immunoglobulin is a special cell contained in a person’s blood that supports his immunity. When foreign cells, viruses or microorganisms are detected, these immune molecules begin to neutralize them.
What is immunoglobulin: features
Immunoglobulins are an important tool of the immune system. They have a number of characteristic features:
- Specificity. It consists of neutralizing exclusively the causative agent of the disease itself. While most antimicrobial and antiviral drugs have a toxic effect not only on pathogens, but also on the body’s own cells.
- Harmless to the body.
- A minimum concentration is required to combat the antigen.
- Mobility. Immunoglobulins travel with the blood to the most distant parts and cells of the body to fight pests.

Functions of immune molecules
Immunoglobulin is a protein that copes with many biological functions, which are as follows:
- recognition of a foreign substance;
- subsequent binding to the antigen and formation of an immune complex;
- protection against re-infection;
- destruction of excess immunoglobulins by anti-idiotypic types of antibodies;
- rejection of tissues of another biological species, for example, transplanted organs.
Classification of immunoglobulins
Depending on the molecular weight, structure and functions performed, five groups of immunoglobulins are distinguished: G (lgG), M (lgM), A (lgA), E (lgE), D (lgD).
Immunoglobulin E (IgE) is found in blood plasma in very small quantities. Fixed on skin cells, mucous membranes and basophils. This group of immunoglobulins is responsible for causing an allergic reaction. Its attachment to the antigen leads to swelling, itching, burning and other allergic reactions.

If immunoglobulin E is elevated, this indicates the penetration of irritating substances into the body or the presence of an allergy to a large number histamines. To establish an accurate diagnosis, additional blood tests should be performed to identify specific antibodies.
Immunoglobulin M (lgM) has an increased molecular weight, which is why it cannot penetrate the child’s blood during his or her intrauterine development. The fetus produces it on its own. The production of this group of immunoglobulins begins first after infection enters the body. Immunoglobulin M plays an important role in the process of removing the pathogen from the bloodstream. An increase in immunoglobulin M is an indicator of a severe inflammatory process in the body. For example, an increased content of these titers indicates the occurrence of an intrauterine infection of the fetus, infection with rubella, syphilis or toxoplasmosis.

Makes up the bulk of immune cells in the blood. Production begins a few days after the infection enters the body and after the production of immunoglobulin M begins. It remains in the body for a long time. This is the only type of antibody that is transmitted from mother to child and creates passive immunity.
Immunoglobulin lgA is called secretory because it protects the respiratory, urinary tract and gastrointestinal tract from infections. It also reflects the attack of viruses on mucous membranes. What immunoglobulin D is, its quantity and functions are still not fully understood.
Prescribing an immunoglobulin test
A blood test to determine the amount of immunoglobulin E is prescribed if bronchial asthma, atopic dermatitis, food or drug allergies are detected. Recurrent pneumonia, skin abscesses, frequent fractures of the limbs, scoliosis and sinusitis indicate a genetic pathology expressed in an abnormally high concentration of group E immune proteins.

An immunoglobulin A test is done for recurrent meningitis, otitis media, sinusitis, myeloma, leukemia, lymphoma.
Deficit state
A deficiency of antibodies of any fraction indicates the presence of an immunodeficiency state. It can be either congenital, that is, primary, or secondary, acquired. This manifests itself in recurrent and chronic bacterial infections. The most common deficiency is immunoglobulin lgA. This is expressed in increased sensitivity to infections. The causes can be very diverse - from nutritional disorders to exposure to ionizing radiation.
Application of human immunoglobulin
Immunoglobulin is not only protein cells that perform a protective function, but also a substance that is actively used in medicine. Available in two forms:
- solution for intramuscular injection;
- powder for
Human immunoglobulin can be prescribed for replacement treatment:
- primary and secondary immunodeficiencies;
- severe viral and bacterial infections;
- various autoimmune diseases;
- AIDS in children;
- for the prevention of diseases in premature infants.
Anti-allergenic immunoglobulin can significantly improve the condition of a child with constantly recurring severe allergies. It can only be prescribed by a qualified attending physician.
Human or animal immunoglobulin can also be found in preventive vaccinations. Serum is used to form passive immunity. Included in vaccinations against influenza, rubella, mumps, and measles.

Treatment with immunoglobulins
Treatment using immune cells is carried out exclusively in a hospital, as there are a number of side effects:
- fever, chills, headaches;
- shortness of breath, dry cough;
- vomiting, diarrhea, stomach cramps;
- drowsiness, weakness, sensitivity to light;
- tachycardia, chest discomfort.
With strict medical supervision, the drug can be prescribed to pregnant women and during breastfeeding.
Where to buy drugs with immunoglobulin
Buy medicinal product with immune cells can be done at the pharmacy. It comes with instructions with detailed description, contraindications and dosage. But you should not buy and take the drug without a prescription. The price of intramuscular immunoglobulin for 10 ampoules averages 800-900 rubles. A 25mm bottle costs an average of 2,600 rubles. You can also purchase medications for emergency prevention, which include human immunoglobulin. Its price will be much higher, but they are simply necessary for a person caught in an epidemic outbreak.

Immunoglobulin is a character, the absence or deficiency of which seriously affects the condition of the human body. Isolated from blood plasma, it is present in most immunostimulating drugs.
Composition and release form of the drug
1 ml (with antibody titer 1:2000) - ampoules (1) - cardboard packs.
1 ml (with antibody titer 1:2000) - ampoules (10) - cardboard packs.
2 ml (with antibody titer 1:1000) - ampoules (1) - cardboard packs.
2 ml (with antibody titer 1:1000) - ampoules (10) - cardboard packs.
pharmachologic effect
An immunologically active protein fraction isolated from human or donor serum tested for the absence of antibodies to HIV (HIV-1, HIV-2), hepatitis C virus and hepatitis B virus surface antigen.
Prevents isoimmunization of a Rho(D)-negative mother exposed to Rh 0 (D)-positive fetal blood at the birth of an Rh 0 (D)-positive child, during abortion (both spontaneous and induced), in the case of amniocentesis, or when receiving injuries to the abdominal organs during...
Reduces the frequency of maternal rhesus immunization when the drug is administered within 48-72 hours after the birth of a fully term Rh 0 (D)-positive child by an Rh 0 (D)-negative mother.
Pharmacokinetics
C max of antibodies in the blood is reached after 24 hours. The half-life of human anti-Rhesus immunoglobulin Rh 0 (D) is 23-26 days. T1/2 of antibodies from the body - 4-5 weeks.
Indications
Drug interactions
Can be used in combination with other drugs (including antibiotics).
special instructions
Children born to women who received human immunoglobulin Rh 0 (D) before birth may receive weakly positive results from direct tests for the presence of antiglobulin at birth. Passively obtained antibodies to Rh 0 (D) can be detected in the mother's blood serum if screening tests for antibodies are performed after prenatal or postpartum administration of human immunoglobulin to Rh 0 (D).
Immunization of women alive should be carried out no earlier than 3 months after the administration of anti-rhesus immunoglobulin.
Drugs in vials and syringes with damaged integrity or markings are not suitable for use, if physical properties(change in color, cloudiness of the solution, presence of unbreakable flakes), if the expiration date has expired, if stored improperly.
If it is determined that the father is Rh 0 (D) negative, there is no need to administer the drug.
After administration of the drug, patients should be observed for 30 minutes. Medical offices must have anti-shock therapies. When anaphylactoid reactions develop, antihistamines, corticosteroids and alpha-adrenergic agonists are used.
The drug is not administered to Rh-positive postpartum women.
Pregnancy and lactation
Used according to indications during pregnancy.