2 dpp five-day cryo sensations. Life after transfer in the IVF program
Development of embryos in the uterus after transfer: what determines the result?
In the IVF protocol, with prolonged cultivation and the absence of natural exit from the membrane, assisted hatching may be recommended
How do embryos behave after transfer?
The presence of “breakdowns” in the genetic material can cause the death of the zygote - (stages of embryo development) - by day - this is the third day after fertilization (the second day of cultivation, since the first day is considered to be zero). Until this time, development occurs by inertia - “on the maternal reserves” of the egg. On the 3-4th day, your own genome comes into play.

The death of the embryo and a stop in the division of blastomeres - a developmental block - most often occurs at this stage, but it also happens later - after transfer, and depends on:
- formed genome;
- the success of switching development processes from “maternal reserves” to one’s own genetic material;
- timeliness of such switching;
- duration of cultivation.
The media used, even the best and most expensive ones, are not the mother’s organism. Long-term cultivation is good, but not in all cases. Doctors are constantly faced with a dilemma: in the first days of development it is difficult, and long-term cultivation can cause development to stop.
Therefore, each individual case is always carefully considered, and then a decision is made on the timing of “growing in an incubator.” The number of resulting embryos, the history of previous attempts and the need for (PGD) are taken into account. This study can be carried out starting from the fourth day of development. Before this period, it is technically difficult to separate the blastomere for research.

Poor-quality genome and cultivation in media are not all the reasons for the death of embryos, but at the initial stages of development they come to the fore. There are also problems related to quality and implantability. Development of embryos after transfer in the early stages, the process is subtle, multifaceted and not fully studied, since it is very difficult to find material to study. Research is still ongoing in this direction.
Let me tell you my story briefly.
My husband and I were unable to get pregnant. Then an independent pregnancy occurred, which ended in a frozen pregnancy at 7-8 weeks. After which they began to thoroughly examine and it turned out that the husband had 100% of the sperm with pathology. They don’t even take eco with this. Treatment was prescribed.
But unfortunately it turned out to be unsuccessful. I was very upset, but it was reassuring that there were 2 embryos left for cryopreservation. True, their quality was, to put it mildly, not very good - 4BB and 3BC. Well, what can I do, don’t throw them away, these are my cells anyway and I need to try all the options.
Then, the next cycle after unsuccessful IVF, I get pregnant on my own. It was a shock for both my husband and my fertility specialist. We were all happy, but at 7-8 weeks the pregnancy stops developing. I was hysterical and had a long depression. I was really tired of all this, procedures, cleanings, pills, tests, etc... it was very difficult mentally. It took me a long time to come to my senses. While I was recovering, we even tried artificial insemination. There is a chance of becoming parents, but it was unsuccessful.
And to be honest, I wasn’t going to move my snowflakes. I was afraid that the pregnancy would be interrupted again. Therefore, I did not even pay for and extend the period of cryopreservation at the Kulakov Scientific Center when my time was up.
So a year passed. And one day they called me from the center and asked if I was going to transfer my embryos? And I asked, do they still exist? And they told me that without my consent they have no right to do anything with them. I was very surprised. And I decided that this was a sign and I had to act.
I came to my fertility specialist and told everything. She used to work in Kulakova, doing eco. Don't be afraid! This is such a chance to become a mother! And now he works in another place. My doctor called the doctor who took me there in Kulakov and said that we wanted to do cryo. She gave the go-ahead. From the 4th day of the cycle, we entered into a cryoprotocol. My successful experience of a cryoprotocol at the Kulakov Scientific Center. It was already fully paid for and did not qualify for compulsory medical insurance. All together it came out to about 30,000 rubles.
I was prescribed medications:
4dc Proginova 1t 2 times a day Builds up the endometrium well. I took it during the cryoprotocol for HRT.
Divigel 1g
Every day I went to Kulakov for an ultrasound and monitored the growth of the endometrium.
15dc prescribed the transfer of 2 embryos. They were successfully defrosted. They were transferred and shown by ultrasound how they were located in the uterus. As support, they also left Proginova, Divigel and added a horse dose of Utrozhestan 800 per day (4 tablets).
I feel nothing at all, not even my chest is swollen and doesn’t hurt.
1 dpp. The next day I went to work. There are no sensations at all.
2 dpp no sensations
3 dpp I started to feel a tug in my stomach like before my period. I was upset and decided that it was a flyover.
4 dpp there are no sensations, the stomach has gone away. The chest is silent.
5, 6, 7 dpp no sensations
8 dpp I couldn’t stand it and took a test and it was POSITIVE! The second fat line appeared immediately.
On 9 dpp I went to Invitro to take an hCG test and it turned out to be 337. Huge! Maybe there are twins?
I called and made my doctors happy. One of them immediately put me on sick leave. I sat on it the entire first trimester.
The first ultrasound revealed that there was only one embryo in the uterus.
I gave birth to him in my native Kulakov Scientific Center. My birth was in the new federal perinatal center at the Scientific Center named after. Kulakova OCTOBER 2016
To summarize, I want to say that the cryoprotocol is much easier to tolerate than a fresh one because it does not require stimulation and puncture.
Pregnancy is no different natural pregnancy, only the support itself was finally canceled at 30 weeks.
Girls, for inspiration I will describe the symptoms in my successful (pah-pah-pah) protocol.
They planted two five-day-olds. What’s interesting is that this time everyone got up and walked from the chair. Just imagine, yeah. No one was taken on a gurney to the ward. And in general they didn’t let me lie down for a second. After the transfer, the girls immediately went down to see the doctor. And everyone was advised to be sure to have a good sex life on the day of the transfer. For blood circulation. Yes, yes, I was shocked too.
I walked from the clinic to the house - the sun was shining, the weather was good - let me, I think, take a walk, since such chaos is happening in the kingdom. Then I read: all this is completely normal - nothing can happen if the cervix is closed. Moreover, when we are in a vertical state, it lies horizontally and the embryos will not go anywhere from there at all.
The temperature rose by 1 DPP and stayed at 37 for two days. I constantly wanted to sleep, I was ready to sleep standing anywhere. There was a metallic taste in my mouth. The breasts have grown sharply (but this is a so-so symptom against the background of progesterone). I started running to the toilet constantly.
My stomach was tugging a little and it’s still tugging (not much, I don’t even drink Noshpa, although the idea flashed through my mind ten minutes ago).
The sleepy state continues to this day. I go to the store to buy food (I haven’t cooked for a week, I don’t have the strength, I can barely drag my feet) - and I’m already tired, I need to sleep for an hour.
I passed the hCG test at 8DPP, but the poet’s soul couldn’t stand it. Showed 281. Most likely, both babies have attached!!! Now I'm waiting for March 9th to take the official test.
Of course, this is all nature, chance, etc. But still I believe that positive attitude helped. There are many studies that show that women who are positive and believe in the results are more likely to become pregnant during IVF. Before the transplant, I specifically worked with my fears (fear of pregnancy, fear of losing my job, and I’m also the unluckiest person in the world, etc.). I reformulated them into positive attitudes and repeated them to myself ten times every day. I ended up with the following attitude: “Getting pregnant is easy and natural. The world loves me and cares about my comfort and well-being. I will be able to bear, give birth and raise healthy children. Nature is wise and she will help me with this.”
I also listened to Sinelnikova’s meditation for pregnant women (it’s on social networks, look it up for anyone who needs it), and fell asleep to it during the day. I drew a visualization picture - a baby in the tummy (I hadn’t even dreamed of two yet) and here my husband and baby are walking on the street - I put it in a frame and hung it on the wall. As I pass by, I will definitely admire it.
Of course, I can only rejoice quietly for now; there are still many stages to go through. But the first result is already there. Here it is, the treasured file in the mail (god, is this all happening to me).
Most of women's knowledge about how pregnancy begins ends at the stage of ovulation and fertilization. Actually, the success or failure of the planning cycle is attributed to the fateful “meeting” of male and female reproductive cells. However, in the matter of developing a new life in a woman’s body, there is another difficult and important point - embryo implantation. In order to increase the personal literacy of planning ladies, this issue should be given special attention.
A little theory
Implementation ovum into the uterus called implantation. The embryonic villi penetrate the lining of the uterus, which may cause minor bleeding.
In order for implantation to be successful, several conditions must be met:
- lush three-layer endometrium with a high content of substances that nourish the embryo;
- high amount of progesterone in the body (so that the embryo can develop and menstruation does not begin);
- normal microflora in the body.
The process of fertilization and development of the fertilized egg- not one-time. And each stage is important for the offensive normal pregnancy and formation of a healthy fetus.
Timing of implantation
After ovulation and the meeting of the egg with the sperm, the fertilized zygote begins to move through the fallopian tubes. Its task is to get into the uterus as quickly as possible in order to gain a foothold in the endometrium specially prepared for this. Along the way, the zygote continuously divides and grows. In progress blastocyte implantation and it happens.
Conventionally, we can distinguish between middle, late and early implantation.
- Early. It is quite rare. Usually, implantation that occurs 6-7 days after ovulation (or 3 dpp - 4 dpp if we are talking about IVF)
- Average. Between fertilization and implantation there are 7-10 days ( embryo implantation after transfer occurs approximately on day 4-5). Doctors say that it takes about 40 hours for Morula to penetrate, after which the body begins to produce the hormone hCG in the blood, which increases basal temperature. Based on this, the so-called embryonic period of development, which lasts until approximately 8 weeks of pregnancy.
- Late. Occurs approximately 10 days after fertilization. This is what always gives women at least a weak, but hope for possible pregnancy- even when you hardly expect it anymore.
If pregnancy does not occur for a long time, then you need to be examined to identify the cause of infertility.

Subjective and objective signs
Both in natural and artificial cycles, women are very excited and want to quickly lift the veil of secrecy - is there a pregnancy or not? They start collecting symptoms and sensations, trying to find some kind of relationship with reality in my well-being. Experts have adopted a simple classification as a basis, according to which all signs can be divided into subjective and objective.
Subjective:
- pulls in the stomach;
- discharge;
- changes in mood, emotional lability;
- tingling in the uterus after ovulation;
- feeling tired, etc.
Girls may even note that after IVF my stomach hurts like before my period. In this case, there is no clear certainty yet, such pain may indicate both the onset of pregnancy due to successful implantation, and the approaching end of the cycle - and the beginning of a new one.
Objective:
- the basal temperature increases after the transfer (after a slight drop in the natural cycle);
- body temperature after transfer may also increase from 37 to 37.9 degrees;
- detection of the hCG hormone in urine and blood.
In this case, it is necessary to distinguish between the levels of pain, the abundance and richness of discharge, and the increase in body temperature. Sometimes what is passed off as signs of fertilized egg implantation, are symptoms of some other disease. If you are in doubt whether your feeling 5 dpo signs fetal implantation or not, it is better to consult a doctor.
Embryo development by day after IVF
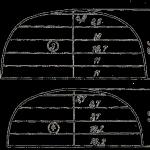
If everything is more or less clear with the natural cycle, then the question is, on what day does embryo implantation occur in a successful protocol? remains open. We present to your attention a daily table:
0 DPP - carry ( cryotransfer)
1DPP- blastocyte emerges from the membrane
2DPP- attachment of blastocytes to the wall of the uterus
3DPP- implantation begins
4DPP- implantation of the morula into the uterus continues
5DPP- end of implantation
6DPP- the placenta begins to produce hCG
7DPP- active growth hCG level
8DPP- HCG continues to rise
9DPP-10 DPP- HCG levels reach the minimum of pregnancy tests
Approximately 11th day ( 11-12 DPP) after the transfer, it is possible to draw conclusions about whether there was successful IVF.

We trust nature
Women re-read tons of literature, trying to find the ones 5 dpo sensation or 6 dpp sensations, which would indicate implantation and, accordingly, the onset of pregnancy. Actually, expectant mothers begin to worry about whether it worked out or not 3 DPO.
This question is equally of concern to girls who have undergone the IVF procedure. Alleged embryo implantation after IVF They try to catch it by minimal changes in the body and well-being. The Internet is replete with queries like “ 5 dpp three days», « 4 dpp of five-day days", « 7 days of five days”, with the help of which women look for positive stories.
It is a bitter disappointment that there is not even a hint of a second page on Day 8 or menstruation after embryo transfer. But in fact, the answer to the question of why doesn't the embryo take root?, there may be an objective situation of natural selection. The non-viable fetus was rejected, giving way to healthy offspring.
In fairness, it is worth noting that if such rejection is repeated constantly, then this is a reason for a complete medical examination. The reason for the failure of a long-awaited pregnancy may be male infertility.
Implantation is a critical point, because the blastocyte is perceived by the woman’s body as a foreign object due to the presence of male genes in the cell. The speedy and successful introduction into the endometrium and the onset of a normal healthy pregnancy depend on how well the defense mechanisms of this cell work.
They say the biggest adrenaline rush isn't the roller coaster, it's waiting for the pregnancy test result. This is especially true for a patient after IVF. The embryo was transferred. A lot has already been accomplished, a lot of effort, time, and money have been spent. There are two weeks of endless waiting ahead...
What happens during this period? The body has already gone through a lot. The prescribed drugs (primarily progesterone and its derivatives) are designed to create optimal conditions for pregnancy. Others, more effective, medicines there is no one for this stage yet. All you have to do is be patient and wait.
At this time, moderate cramping pain, scant bloody issues or even light bleeding, slight bloating, general fatigue and breast tenderness. Symptoms should not get worse. Their presence (as well as absence) does not mean that pregnancy has not occurred.
Please note that if, after completing an IVF program, you experience excessive, increasing abdominal bloating and tenderness, shortness of breath, chest pain, or difficulty urinating, you should urgently contact your clinical team as these are the first signs of hyperstimulation syndrome and intensive care will likely be required.
But even if everything is fine, painful doubts and premonitions do not leave:
Please tell me, does the absence of discharge or any other symptoms indicate that implantation has not taken place again?? Today I have the 3DPP of two five-day days, according to the timing it should already happen. For the first 2 days my lower abdomen ached, today I feel like an astronaut. I’m very worried that there are NO sensations AT ALL…….
Help with advice: transfer of 3 blastocysts good quality. here is my hCG 5DPP - 2.8 (I already decided that the flight and all the appointments were carried out mechanically), 12DPP - 118.8 (I was very surprised), 14DPP 253.1. To the table hCG norms I can't fit in. what can be done to pull the baby out? This is already the 8th transfer.
Please tell me, if at 7 DPP of three days the hCG is negative, can we hope for pregnancy?
Questions like this come up often. In this regard, I would like to talk a little more about the early diagnosis of pregnancy, how hCG grows, and whether it is worth making any predictions based only on its values. Are laboratory tests of hormone levels and blood coagulation parameters justified at this stage?
 I'll start with the main thing: hCG (human chorionic gonadotropin)- a special pregnancy hormone. It is an important indicator of the development of pregnancy and its deviations. Human chorionic gonadotropin is produced by cells of the germinal membrane immediately after its attachment to the wall of the uterus (implantation). Based on the obtained figure, the doctor determines the presence of fetal tissue in the body, and therefore the onset of pregnancy in the woman.
I'll start with the main thing: hCG (human chorionic gonadotropin)- a special pregnancy hormone. It is an important indicator of the development of pregnancy and its deviations. Human chorionic gonadotropin is produced by cells of the germinal membrane immediately after its attachment to the wall of the uterus (implantation). Based on the obtained figure, the doctor determines the presence of fetal tissue in the body, and therefore the onset of pregnancy in the woman.
Level blood hCG can be detected as early as 6–8 days after implantation, which suggests the onset of pregnancy (the concentration of hCG in the urine depends on the sensitivity of the test and usually reaches the diagnostic level 1–2 days later than in the blood serum). It is worth noting that the timing of the appearance of the first positive hCG values and the rate of its increase are similar, but in 15% of cases they do not fit into generally accepted norms and require more careful monitoring to make a correct diagnosis.
In 85% of cases normal course of pregnancy, between 2 - 5 weeks, accompanied by a doubling of hCG every 72 hours. The peak concentration of hCG occurs in the 10th - 11th week of pregnancy, then its concentration begins to slowly fall. This is the result of the work of the “embryo-placenta” complex; it is the placenta that begins to independently maintain the necessary hormonal levels. By this time, the body no longer needs a high level of hCG.
Increased levels of human chorionic gonadotropin during pregnancy can occur with:
normal intrauterine pregnancy(individual characteristics in 10 - 15%)
- multiple pregnancy
- toxicosis
- mother's diabetes
- some genetic pathologies of the fetus
- trophoblastic disease
- incorrectly determined gestational age
- taking synthetic gestagens (drugs from the progesterone group)
Its elevated values can also be seen within 7-10 days after a terminated pregnancy (medical or spontaneous abortion). But the concentration of hCG in dynamics in these cases does not increase, but more often falls.
Low human chorionic gonadotropin levels may indicate incorrect timing of pregnancy or be a sign of serious disorders, such as:
- ectopic pregnancy
- non-developing pregnancy
- delayed fetal development
- threat of spontaneous abortion
- some other rarer conditions.
It is important to understand that a decrease in the hCG value in repeated studies indicates only one thing: the development of the fertilized egg has already stopped, it is impossible to resuscitate it. The exception is a laboratory error (not often, but it happens).
Optimal time frame for determining hCG levels 12-14 days after transfer(lower chance of error). If a two-week wait is insurmountable for you, you can donate blood earlier, starting from day 7-8, but having received any (positive or negative) value, do not draw conclusions until you repeat the analysis 2-3 times over time.
HCG values depending on the stage of pregnancy are in many laboratory tables, I will not repeat them here. But it is important to consider the following:
- From 0 to 10.0 mIU/ml on days 13-14 after transfer - no pregnancy.
- From 10.0 to 25.0 mIU/ml is a questionable value that requires repeating; the presence of implantation is controversial.
- From 25.0 mMEml and above is a positive value, an indicator of implantation.
- When examined on the 16th day after puncture, the level of hCG in the blood above 100 mIU/ml (for embryos of the 3rd day) or 130 mIU/ml (for embryos of the 5th day) indicates a high chance of successful development of pregnancy, while While at lower values, the probability of intrauterine progressive pregnancy is not high.
- Any positive hCG number dictates the need retain previously assigned support, primarily progesterone preparations (Crinone, progesterone, utrozhestan, duphaston and others). In controversial cases (the figure is below the statistical average, there is bloody discharge from the genital tract, etc.), it is necessary to plan repeated determinations of hCG every 4-5 days. With an increase in the hCG value, we can clearly speak of a progressive pregnancy, but an ectopic pregnancy cannot be excluded.
- With a progressive decrease in hCG levels, maintaining maintenance therapy is not worth it. This will only increase the time of uncertainty and vain hopes. The most common causes of undeveloped pregnancy are genetic disorders of the fetus. As a rule, it is not possible to save a pregnancy with severe genetic abnormalities. And is it worth it? Cancellation of maintenance therapy should be discussed with your gynecologist.
- More specific information about the onset of pregnancy can only be provided by Ultrasound of the pelvic organs, which can be planned no earlier than 20-22 days after the transfer.
- The dynamics of the increase in hCG can only be assessed when lack of support for hCG-containing drugs(pregnyl, human chorionic gonadotropin, choragon and others). Trace concentrations of externally administered hCG remain for 5 to 15 days. depending on the dose received and individual characteristics body. A sufficient number of studies have been published indicating that the use of these drugs does not affect the prognosis, but makes it much more difficult to assess the results obtained.
- The hCG level after a 5-day embryo transfer is often slightly higher than after a 3-day embryo transfer, and practically does not depend on whether the transfer was fresh or cryo.
Another “fashionable topic” - control of blood hormone levels in the period after the transfer for the purpose of adjusting support medications.
I want to get a consultation, I have 18dpp, hCG 970, support: duphaston 2 tab 3 times a day, Divigel 2 g. Folio, I tested estradiol - 725, progesterone -15.6... Tell me, is there enough support? Are your hormones normal?
***
Help me understand, 3 dpp blastocyst, today I tested progesterone 105.0 nmol/l (1 trim: 29.6 - 106), estradiol 68 pmol/l. In ingest support 2.5.% 2 rub. per day, kraynon at night, proginova 0.5 tablets per day. Is estradiol low? Perhaps we need to increase our support for progynova?
The initial idea looked logical: you determine the level of hormones (progesterone and estrogens) in the blood and, knowing their norms, adjust medication prescriptions, like on a scale, adding a deficiency. These recommendations have existed in many guidelines for some time. But in practice everything turned out to be much more complicated.
Firstly, laboratory values of hormone levels during repeated studies in the blood vessel and in the uterine vessels (obtained during surgery) turned out to be different. The concentration of hormones in the uterine tissue was much higher.
Secondly, the production of hormones is pulsating. One secretory impulse takes from 60 to 90 minutes. Shouldn’t we take analysis multiple times throughout the day to calculate average concentrations?
Thirdly, the level of hormones is additionally maintained by vaginal forms of gestagens, which have a slightly different chemical formula than the progesterone we know. That is, they are present in the blood, but are not detected in the analysis (another formula).
Therefore, laboratory testing of progesterone levels has limited clinical value because does not reflect his true concentration in the uterine vessels and n is not a reason to change support. It is impossible, looking at the calm surface of water near the shore, to estimate the speed of the river flow in the fairway.
At later stages of pregnancy, when the fetus-placenta complex comes into play, the concentration of progesterone can be one of indirect signs progression of intrauterine pregnancy. But by this time, more reliable information can be obtained during an ultrasound scan.
Determining estrogen levels to assess chances of pregnancy is even less promising. A high concentration of estrogen in the blood only indicates the severity of the hyperstimulation syndrome. There is no correlation between estrogen levels and pregnancy rates. In addition, the introduction of external estrogens in the period after the transfer is not always justified.
I’ll write a little more about the myth of “ thick blood«:
I had a transfer of 2 five-day-old blastocysts. On the third day after the transfer, I took a D dimer test, the result was 2121.6 ng/ml!!! And on the fourth I passed the RFMC, the result was 12 mg/dl (normal range 0.00-4.00). I inject fraxiparine 0.3 2 times a day and take thromboass 100 mg. Please tell me, is it possible to indirectly assume from such indicators that implantation has occurred? And why are such high rates dangerous?
Please tell me how often do I need to monitor D dimer after the transfer? And in general, is it advisable to do this? For some reason, doctors have a mixed opinion about high rates... Some say that this is normal... Others say that it is necessary to urgently change therapy, that this is very dangerous...
The opinions of doctors in assessing this factor are indeed ambiguous. In different clinics you can hear directly opposite recommendations on the significance of altered hemostasis parameters in the ART protocol. This creates confusion, misunderstanding, who is right, is it important to “monitor hemostasis” after the transfer? Does the administration of low molecular weight fraxiparins affect the final result?
There are always controversial topics in science. This is one of them. I am close to the position that fluctuations in some values of the coagulation system do not influence the onset of pregnancy. Increasing a number of indicators of the hemostatic system is a kind of “patches” for the repair of blood vessels and protection against obstetric hemorrhage.
Studies show that the incidence of thrombophilia among women requiring IVF is the same as among absolutely healthy women - about 7%. During IVF in women with thrombophilia, the birth rate was the same (60.8% after 6 cycles) as in women without thrombophilia (56.8% after 6 cycles) - this means that testing for thrombophilia before IVF is not informative, detection and treatment of thrombophilia during IVF does not affect the prognosis. In addition, many external factors can contribute to “hemostasis disorders”: ovulation stimulation, follicle puncture, onset multiple pregnancy and much more. Today there are no absolute norms for coagulogram indicators for different conditions (except for assessing basic indicators outside stimulation and pregnancy). In this connection, I am sure that “monitoring hemostasis” and prescribing expensive fraxiparins most likely has only commercial interest.